Internal Medicine IV
Research Focus
General Facts
Research
Selected Publications
Selected Funding, Collaboration
Devices & Services
Keywords: Chronic kidney disease; immune mediated kidney disease; haemodialysis; renal transplantation; systems biology; in silico disease modelling; precision medicine; epidemiology
Research (ÖSTAT Classification) : 30205
Research Focus
- Precision medicine: The prognosis of patients with renal disease has improved. Yet, inter and longitudinal intra-individual response to therapy is variable and a better understanding will optimise individual clinical management.
- Epidemiology: The Austrian Dialysis and Transplant Registry collects data from patients with end-stage renal disease. Understanding the epidemiology will provide information on the effectiveness of ESRD and pre-ESRD therapy and will support healthcare planning .
General Facts
The Department of Internal Medicine IV (Nephrology and Hypertension) is the primary service provider for Tyrol and the tertiary referral centre for Western Austria and Southern Tyrol for patients with renal diseases and difficult-to-control hypertension (catchment area: ~2 million). We offer an outpatient clinic, an inpatient ward, a dialysis centre, and a routine and research laboratory. As well as caring for patients with chronic kidney disease and transplant recipients, the outpatient clinic provides special consultations for autoimmune diseases, rare diseases and the diagnostic work-up/treatment of refractory hypertension. The 18 members of the medical staff perform state-of-the-art sonography and around 100 renal biopsies per year. Ambulatory dialysis patients are treated in collaboration with a local dialysis provider unit and by the peritoneal dialysis programme of the department (CAPD, APD and assisted PD service). The in-house dialysis unit takes care of patients with end-stage as well as acute renal failure as well as offering liver replacement therapy, plasmapheresis and immune apheresis for renal, haematological or neurological autoimmune diseases, antibody-mediated transplant rejection and ABO-incompatible renal transplantation. In collaboration with the Department of General and Transplant Surgery, the Innsbruck transplant programme offers care for renal transplant living donors and recipients, with 120 – 150 transplants per year.
Research
Precision Medicine in Chronic Kidney Disease (CKD)
DKD: Simone Schmid, Sara Denicolo, Stefani Thöni, Felix Keller, Susanne Eder, Johannes Leierer, Paul Perco, Markus Pirklbauer, Gert Mayer
CKD: Julia Kerschbaum, Hannes Neuwirt, Michael Rudnicki
Immune-mediated kidney disease: Philipp Gauckler, Andreas Kronbichler
The prognosis of CKD has improved dramatically over the last decade, as new treatment options have become available. Following large interventional studies, updated guidelines have been published with the aim of improving the standard of clinical care in patient cohorts. However, on an individual level, the clinical trajectory and response to therapy of CKD show marked cross-sectional inter and longitudinal intra-individual variability. Supported by several European Union grants (Syskid, Beat-DKD, DC-ren, PERSTIGAN), the research focus of the department is on approaches to the implementation of precision medicine in various CKD settings.
- Diabetic kidney disease (DKD): It has become obvious that renal impairment in patients with diabetes mellitus is a complex phenotype with heterogenous prognosis and response to therapy. Computational systems biology using multi-omics data and advanced disease-modelling techniques (such as the application of dynamic systems theory tools) are employed to offer better understanding and description of the clinical course, pathophysiology and response to therapy of DKD on an individual clinical and molecular level. The major aims are:
(i) To decipher intrinsic reno-protective mechanisms and identify novel therapeutic targets,
(ii) To identify and apply prognostic and predictive biomarkers/biomarker panels in clinic,
(iii) To investigate drug mechanisms of action in relation to disease pathophysiology.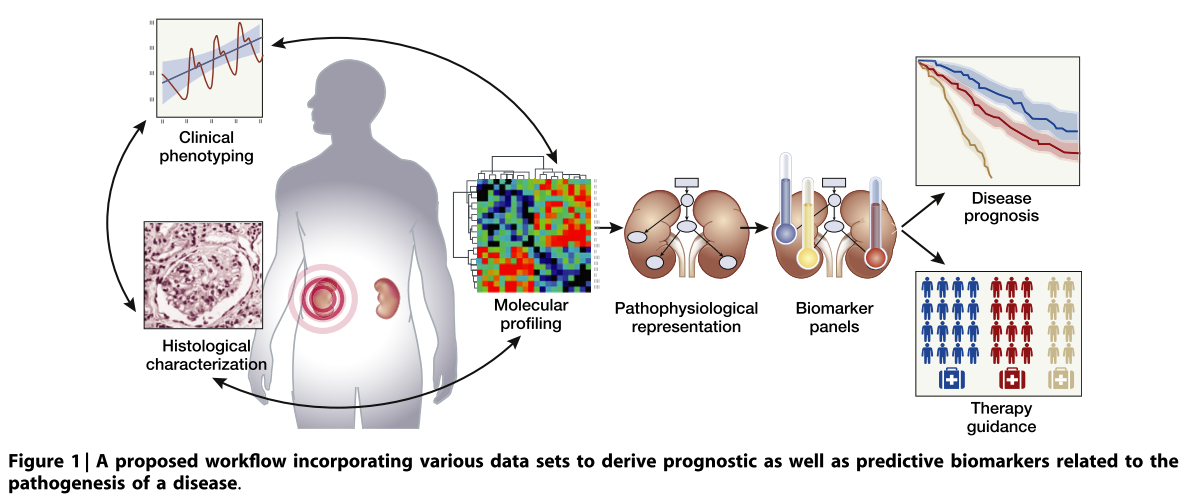
Fig. 1: Systems biology data integration allows pathophysiological disease modelling to delineate biomarkers for disease prognosis and therapy guidance.
In line with these efforts, the Innsbruck Diabetic Kidney Disease Cohort was initiated. Patients with early renal dysfunction undergo a kidney biopsy to assess the individual histopathological phenotype and this is supported by an extensive biobanking effort over a follow-up period of five years. This complements the repository of the prospective observational international cohort study PROVALID recruited 4,000 patients with type 2 diabetes mellitus, with follow-up of at least four years. - IgA Nephropathy: Kidney function decline in IgA nephropathy (IgAN) can be significant and is not predictable using the available clinical and histological tools. The EU/FWF-funded programme PERSTIGAN identified a urinary biomarker-based classifier (IgAN237), which showed significant added value for the prediction of disease progression compared with the clinical parameters (age, gender, proteinuria, eGFR, mean arterial pressure). This proteomic supported panel is available as an online risk calculator (www.perstigan.eu) and is undergoing further evaluation of its potential to guide treatment decisions in a prospective clinical trial.
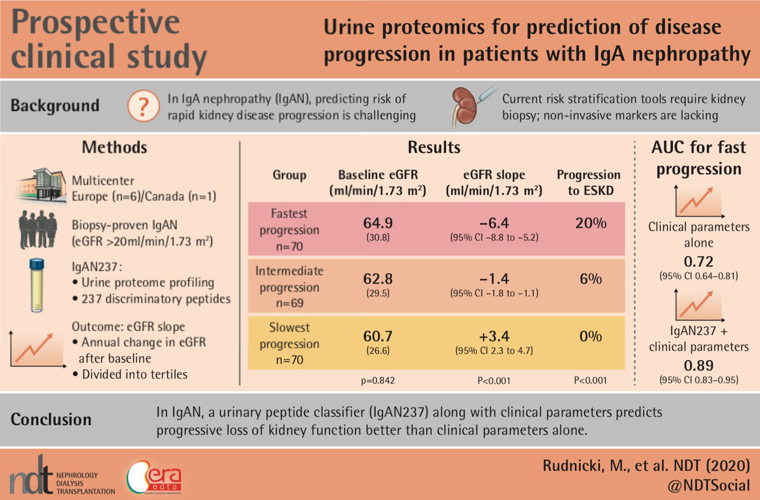
Fig. 2: Visual abstract of the PERSTIGAN project. - Immune-mediated kidney disease: The pathogenesis of immune-mediated kidney disease is still poorly understood. A recent study found that, among the microbiota of patients with granulomatosis with polyangiitis (GPA), the presence of aureus was more abundant and, for the first time, the relationships of S. epidermidis, S. pseudintermedius and S. aureus were described as antagonistic to one another.
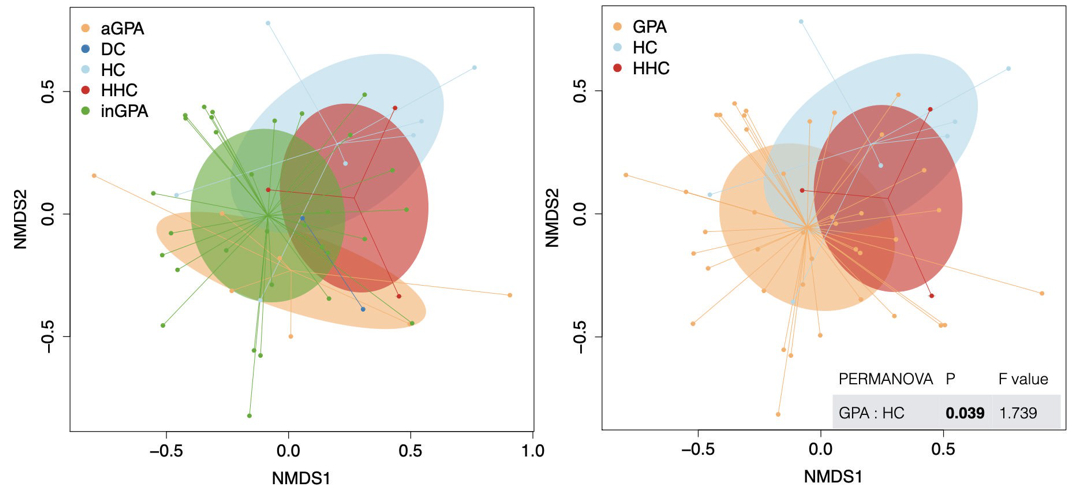
Fig. 3.: NMDS analysis of bacterial 16S marker gene sequenced species. a) The healthy control cluster separates the majority from the inactive and active GPA cluster. b) The GPA cluster (including active and inactive cases) was statistically different from the healthy control cluster.
Ongoing research is focusing on diagnosis, prognosis and therapeutic regimen to improve overall prognosis of patients with autoimmune kidney diseases. As such, the research pipeline was extended to COVID-19 and established the COV-GN registry. This registry aims to collect data from centres around the globe (from Japan to Brazil) on how COVID-19 infections have affected short and long-term prognosis and to provide information on treatment of the infection and glomerular disease. Other international projects are focusing on treatment response variability in ANCA-associated vasculitides and nephrotic diseases. - Haemodialysis:
Patients on renal replacement therapy suffer from excessive cardiovascular morbidity and mortality. The assessment of individual calcium kinetics during dialysis serves as an example for the study of individual heterogeneity in response to fixed, guideline-recommended dialysis prescription in a population. - Renal transplantation:
Individual adaption of immunosuppressive therapy is crucial for long-term transplant as well as recipient survival. Research is focusing on immune surveillance using torque teno virus-guided therapy and optimised selection of drug combinations. In collaboration with the Department of General, Visceral and Transplant Surgery, work on an ex vivo organ perfusion system is ongoing.
The Austrian Dialysis and Transplant Registry (ÖDTR)
Karin Gillich, Franziska Engler, Julia Kerschbaum, Gert Mayer
Since the 1960s, the Austrian Dialysis and Transplant Registry has collected individual data on all patients with end-stage renal disease who require dialysis or kidney transplantation. Since its move to Innsbruck in 2018, the registry has undergone transformation into web-based data repository, following rules set out in GDPR. The ÖDTR supports national healthcare authorities in the planning of regional dialysis facility resource allocation. In addition, it provides various quality-control programmes of the Austrian Society of Nephrology. Because of the high quality and completeness of the data collected, the registry is also an outstanding source for academic research. In addition to internal projects, the ÖDTR collaborates with national and international researchers and organisations (such as the European Renal Association – European Dialysis and Transplant Association) under the guidance of an external advisory board.
Selected Publications
- Perco P; Ju W; Kerschbaum J; Leierer J; Menon R; Zhu C; Kretzler M; Mayer G: Rudnicki M; Nephrotic Syndrome Study Network (NEPTUNE): Identification of dicarbonyl and L-xylulose reductase as a therapeutic target in human chronic kidney disease. JOURNAL OF CLINICAL INVESTIGATION INSIGHT. 2019; 4: e128120.
- Mayer GJ; Wanner C; Weir MR; Inzucchi SE; Koitka-Weber A; Hantel S; von Eynatten M; Zinman B; Cherney DZI: Analysis from the EMPA-REG OUTCOME trial indicates empagliflozin may assist in preventing the progression of chronic kidney disease in patients with type 2 diabetes irrespective of medications that alter intrarenal hemodynamics. KIDNEY INTERNATIONAL. 2019; 96; 489-504.
- Heerspink HJL, Perco P, Mulder S, Leierer J, Hansen MK, Heinzel A, Mayer G: Canagliflozin reduces inflammation and fibrosis biomarkers: a potential mechanism of action for beneficial effects of SGLT2 inhibitors in diabetic kidney disease. 2019; 62; 1154-1166.
- Kerschbaum J; Rudnicki M; Dzien A; Dzien-Bischinger C; Winner H; Heerspink HL; Rosivall L; Wiecek A; Mark PB; Eder S; Denicolò S; Mayer G: Intra-individual variability of eGFR trajectories in early diabetic kidney disease and lack of performance of prognostic biomarkers. SCIENTIFIC REPORTS. 2020; 10, 19743.
- Kerschbaum J; Bitter S; Weitlaner M; Kienzl-Wagner K; Neuwirt H; Bösmüller C; Mayer G; Schneeberger S; Rudnicki M: Arterial hypertension as a risk factor for reduced glomerular filtration rate after living kidney donation. JOURNAL OF CLINICAL MEDICINE. 2020; 9; 338.
- Rudnicki M; Siwy J; Wendt R; Lipphardt L; Koziolek MJ; Maixnerova D; Peters B; Kerschbaum J; Leierer J; Neprasova M; Banasik M; Sanz AB; Perez-Gomez MV; Ortiz A; Stegmayr B; Tesar V; Mischak H; Beige J; Reich HN on behalf of the PERSTIGAN working group: Urine proteomics for prediction of disease progression in patients with IgA nephropathy. NEPHROLOGY DIALYSIS & TRANSPLANTATION. 2020 in press
- Koppelstaetter C; Leierer J; Rudnicki M; Kerschbaum J; Kronbichler A; Melk A; Mayer G; Perco P: Computational drug screening identifies compounds targeting renal age-associated molecular profiles. COMPUTATIONAL AND STRUCTURAL BIOTECHNOLOGY JOURNAL. 2019; 17; 843-853.
- Gauckler P; Bettac EL; Nairz M; Duftner C; Luger AK; Stein M; Wanner D; Böckle BC; Tiefenthaler M; Schratzberger P; Neuwirt H; Harasser L; Mayer G; Kronbichler A: What comes after the lockdown? Clustering of ANCA-associated vasculitis: single-centre observation of a spatiotemporal pattern. ANNALS OF THE RHEUMATIC DISEASES. 2020 doi: 10.1136/annrheumdis-2020-219212. Online ahead of print.
- Kronbichler A; Gauckler P; Windpessl M; Shin JI; Jha V; Rovin BH; Oberbauer R: COVID-19: implications for immunosuppression in kidney disease and transplantation. NATURE REVIEWS IN NEPHROLOGY. 2020; 16, 365-367.
- Kronbichler A; Leierer J; Shin JI; Merkel PA; Spiera R; Seo P; Langford CA; Hoffman GS; Kallenberg CGM; St Clair EW; Brunetta P; Fervenza FC; Geetha D; Keogh KA; Monach PA; Ytterberg SR; Mayer G; Specks U; Stone JH; RAVE−ITN Research Group: Association of pulmonary hemorrhage, positive proteinase 3, and urinary red blood cell casts with venous thromboembolism in antineutrophil cytoplasmic antibody-associated vasculitis. ARTHRITIS&RHEUMATOLOGY. 2019; 71:1888-1893.
- Pirklbauer M; Fuchs L; Heiss R; Ratschiller T; Mayer G: Intradialytic calcium kinetics and cardiovascular disease in chronic hemodialysis patients. BLOOD PURIFICATION. 2020; 49; 723-732.
- Pirklbauer M; Bernd M; Fuchs L; Staudinger P; Corazza U; Leierer J; Mayer G; Schramek H: Empagliflozin inhibits basal and IL-1β-mediated MCP-1/CCL2 and endothelin-1 expression in human proximal tubular cells. INTERNATIONAL JOURNAL OF MOLECULART SCIENCE. 2020; 21, 8189
- Pirklbauer M; Schupart R; Fuchs L; Staudinger P; Corazza U; Sallaberger S; Leierer J; Mayer G; Schramek H: Unravelling reno-protective effects of SGLT2 inhibition in human proximal tubular cells. AMERICAN JOURNAL OF PHYSIOLOGY RENAL PHYSIOLOGY. 2019; 316; F449-F462.
- Kronbichler A; Effenberger M; Shin JI; Koppelstätter C; Denicolò S; Rudnicki M; Neuwirt H; Soler MJ; Stevens K; Bruchfeld A; Tilg H; Mayer G; Perco P: Is there decreasing public interest in renal transplantation? A Google TrendsTM JOURNAL OF CLINICAL MEDICINE. 2020 9:1048
- Neuwirt H; Leitner-Lechner I; Kerschbaum J; Ertl M; Pöggsteiner F; Pölt N; Mätzler J; Sprenger-Mähr H; Rudnicki M; Schratzberger P; Eder IE; Mayer G: Efficacy and safety of belatacept treatment in renal allograft recipients at high cardiovascular risk-a single center experience. JOURNAL OF CLINICAL MEDICINE. 2019; 8; 1164
- Jager KJ; Kramer A; Chesnaye NC; Couchoud C; Sánchez-Álvarez JE; Garneata L; Collart F; Hemmelder MH; Ambühl P; Kerschbaum J; Legeai C; Del Pino Y; Pino MD; Mircescu G; Mazzoleni L; Hoekstra T; Winzeler R; Mayer G; Stel VS; Wanner C; Zoccali C; Massy ZA: Results from the ERA-EDTA Registry indicate a high mortality due to COVID-19 in dialysis patients and kidney transplant recipients across Europe. KIDNEY INTERNATIONAL. 2020; 98, 1540-1548.
- Watschinger B; Watschinger C; Reindl-Schwaighofer R; Meyer EL; Deak AT; Hammer T; Eigner M; Sprenger-Mähr H; Schneeberger S; Cejka D; Mayer G; Oberbauer R; Rosenkranz AR; Kerschbaum J: Impact of timely public health measures on kidney transplantation in Austria during the SARS-CoV-2 outbreak-a nationwide analysis. JOURNAL OF CLINICAL MEDICINE. 2020; 9, 3465.
- Pippias M; Jager KJ; Åsberg A; Berger SP; Finne P; Heaf JG; Kerschbaum J; Lempinen M; Magaz Á; Massy ZA; Stel VS: Young deceased donor kidneys show a survival benefit over older donor kidneys in transplant recipients aged 20-50 years: a study by the ERA-EDTA Registry. NEPHROLOGY DIALYSIS & TRANSPLANTATION 2020; 35; 534-543.
Selection of Funding
Grant Support:
- Markus Pirklbauer: Österreichische Nationalbank Anniversary Fund (grant number 18362): Intradialytic calcium kinetics and cardiovascular risk in hemodialysis patients
- Andreas Kronbichler: NIH/NIAID Immune Tolerance Network (EIN No. 81-0726604)
- Michael Rudnicki: ERA Per Med: PERSTIGAN ( No. ERAPERMED 2018-217)
- Gert Mayer: Innovative Medicines Initiative (grant number 115974): Biomarker enterprise to attack diabetic kidney disease (Beat-DKD)
- Gert Mayer: Coordinator: Horizon 2020 (grant number 848011): Drug combinations for rewriting trajectories of renal pathologies in type II diabetes mellitus (DC-ren)
Collaborations
- Heerspink Hiddo, University Medical Center Groningen, The Netherlands
- Ibberson Mark and Burdet Frederick, Swiss Institute of Bioinformatics, Lausanne, Switzerland
- Jayne David, University of Cambridge, United Kingdom
- Kotanko Peter, Renal Research Institute, New York, USA
- Kretzler Matthias and Ju Wenjun, University of Michigan, Ann Arbor, USA
- Lancet Doron and Fishilevich Simon, Weizmann Institute of Science, Rehovot, Israel
- Mayer Bernd and Lukas Arno, emergentec biodevelopment GmbH Vienna, Austria
- Mischak Harald, Mosaiques Diagnostics GmbH, Hannover Germany
- Oberbauer Rainer and Heinzel Andreas, Medical University of Vienna, Vienna, Austria
- Poli Irene and Silvestri Claudio, European Center for Living Technology, Ca` Foscari University of Venice, Venice, Italy
- Rossing Peter, STENO Diabetes Center, Copenhagen, Denmark
- Stone John, Massachusetts General Hospital, Boston, USA
Devices & Services
- The Department has established a biobank of several hundred thousand samples of different body fluid matrices and kidney biopsies. The patients included suffer from CKD, DKD and end stage renal disease (dialysis and transplantation).
- We execute mRNA microarray protocols for large-scale analysis of gene-expression in various samples. Genome wide gene expression profiling is combined with state-of-the-art methods such as qPCR, immunohistology, in situ hybridization, western blotting and ELISAs to evaluate candidate genes and proteins using equipment like GenePix 4000B, Quantstudio 5, Olympus VS120 or Tecan Reader.
- We manipulate in vitro gene- and protein expression, respectively, using CRISPR/Cas to analyse cellular functions.
- We use state of the art bioinformatics tools to analyse expression profiles and run network/network interference analysis.
 Univ.-Prof. Dr.med.univ. Gert Mayer
Univ.-Prof. Dr.med.univ. Gert Mayer
Director
Contact:
Anichstraße 35
6020 Innsbruck
Austria
Email: gert.mayer-med.ac.at
Phone: +43 512 504 25855
Fax: +43 512 504 25857
https://nephrologie.tirol-kliniken.at/



