Orthopaedics and Traumatology
Research Focus
General Facts
Research
Selected Publications
Selected Funding, Collaboration
Devices & Services
Keywords: Clinical studies, biomechanics, fracture fixation, cell biology, osteoporosis, geriatric patients, Orthopaedics, medical microbiology, implantrelated infections, minimal-invasive surgery, biomedical engineering, arthroplasty, tumor, oncology
Research (ÖSTAT Classification) : 106049, 211904, 302019, 302085, 305908, 302057, 303020, 301902, 302048, 206001
Research Focus
Research in the Department of Orthopaedics and Traumatology focuses on the evaluation, development, innovation and improvement of new and existing treatments and therapies for traumatic and degenerative musculoskeletal diseases. We focus on daily challenges and difficulties and try to solve them and find answers through research, conducting prospective randomised studies for high-level evidence and retrospective studies for quality control with the support of the study coordination unit, and initialising biomechanical cadaver tests to improve implant behaviour and find solutions to joint instabilities. To improve our clinical results, we use navigation and robotics in joint arthroplasty. Our interdisciplinary focus is on orthopaedic and trauma-related infection and implant migration to prevent and treat infection. As a reference centre for orthopaedic tumour treatment, we have a large number of patients, which means that we are also able to conduct research in this field. We are proud to have a morphology and cell biology laboratory, the experimental orthopaedics unit and the micro-CT core facility, which enable us to conduct high-level research. The digital operating room is increasingly becoming a reality, with newly emerging technologies such as augmented reality and robotic-assisted surgery for future research.
General Facts
In the routine clinical setting, the department is organised into teams that specialise in anatomical regions. The clinical patient-based research as well as the applied and basic research of all the clinical teams in the department is supported by the aforementioned, interconnected infrastructure and this facilitates a broad spectrum of research. This setting supports both clinical research and laboratory research at macroscopic, microscopic and cellular level.
Clinical research in orthopaedics and traumatology represents a special challenge, because of its high throughput of in-patients and outpatients and its wide range of treatment modalities.
The research fields of medical device studies and investigator-initiated trials explore new treatment methods (basic research). The study coordination team supports the researchers with the planning, organisation and implementation of the clinical trials.
In the biomechanics laboratory, materials testing machines are available for in vitro testing of soft and hard biological tissues, with several custom-made test setups for various anatomical regions as well as joint simulators for the spine, knee, shoulder and hand. These allow in vitro functional evaluation of interventional surgical procedures for the stabilisation or reconstruction of joints as well as soft and hard tissue. Research projects have been conducted in collaboration with internal and external academic partners and with MedTech Industry.
The orthopaedic biomechanical gait laboratory deals with movement analysis and movement optimisation. A Lucotronic system is used to analyse everyday movements and to gather important information for the improvement of ergonomic behaviour.
The main focus of the morphological/cell biological laboratory is on intervertebral disc cell (IVD) investigations and specifically on traumatised IVDs and IVDs from patients with a degenerative disc disease. Moreover, the study of aging processes provides further insights in post-traumatic changes and differences from disc degenerative diseases. Osteoporosis and its underlying mechanisms have also been studied in a fully equipped tissue culture unit. Research projects have been conducted in collaboration with Histology and Embryology, the Department of Radiology and several groups from the CCB.
The experimental orthopaedics unit is a research department within the Department of Orthopaedic and Trauma Surgery at Innsbruck Medical University. The unit is divided into two major research areas: biomedical engineering (which focuses on improving techniques for filling bone defects and on bone removal in the field of orthopaedics) and implant-related infections (with studies that aim to understand biofilm formation and attachment on biomaterial surfaces).
The core facility of micro-computed tomography (micro-CT) is equipped with two micro-CT scanners (vivaCT40/Scanco Medical and XtremeCT II/Scanco Medical) operated in cooperation with the University Hospital for Radiology.
Research
Clinical Research – Study Coordination
Mariette Fasser, MSc
We provide support with the organisation and administration of clinical trials, ensuring study planning and implementation in accordance with local and international legal requirements. Furthermore, the study coordination team also manages funding aspects, ethics submissions, contract tracing and internal registrations.
In recent years, the focus of clinical studies in orthopaedics and traumatology has no longer been limited to medical device investigations; expansion to interdisciplinary projects and further aims became possible as a result of greater experience and knowledge. This facilitated successful participation in EU and FWF-funded trials and opened doors to evidence-based medicine on a high level. The recently completed D.A.CH. project in collaboration with ETH Zürich on the local remodelling of bone fracture healing in healthy, elderly, osteoporotic people with HR-pQCT represents one example. In addition, secondary hip fracture prophylaxis remains an important medical focus, which will be investigated within a drug administration trial with pharmaceutical sponsor AgNovos Healthcare. Interdisciplinary collaboration with the Institute of Hygiene and Medical Microbiology concentrates on the reduction of bacteria by means of sodium chlorotaurine, which was approved by the Tyrolean Science Fund this year.
However, the main research focus recently remains on musculoskeletal topics, e.g. the fixation and treatment of distal radius and proximal humerus fractures, fracture reduction in implant failure and steps to prevent fixation failure, the improvement of spinal cord injury treatment, the treatment of benign and malign musculoskeletal tumours, knee arthroscopy, and primary as well as revision joint arthroplasty.
Biomechanics Laboratory
Werner Schmölz, Assoc. Prof., PhD, Dipl. Ing (FH)
Implant anchoring in stabilisation procedures in patients with reduced bone quality still poses a challenge to surgeons. New test setups, loading protocols and algorithms to detect implant loosening during dynamic loading were therefore developed and applied. Using these developed tools, implant anchoring was investigated in various anatomical regions for different augmentation techniques and augmentation materials. Among others, we developed a technique for screw-tip augmentation with PMMA for calcaneus fractures and successfully demonstrated a significant improvement with the new technique. For spinal procedures, we investigated different implant and vertebra-augmentation techniques. Because of the potential negative effects of PMMA as an augmentation material, we investigated an injectable, medical-grade silicone for pedicle screw augmentation and discovered that it produced greater resistance to implant loosening than PMMA under dynamic load and could be used as an alternative augmentation material. In cooperation with Medtech Industry, we tested a novel technique to reinforce pedicle screw anchoring with an ultrasound-melted, resorbable polymer.
As an alternative to metallic implants, we investigated carbon fibre reinforced PEEK implants for spinal stabilisation procedures. In our experiments, CF/PEEK pedicle screws and vertebral body replacements showed pedicle screw anchoring and segmental stabilisation comparable with conventional metal alloy implants, whilst having the advantage of producing fewer artefacts in CT and MRI imaging.
To improve instrumentation for cervical and lumbar spinal fusion procedures, in vitro experiments were conducted to investigate the primary and secondary stiffness of various supplementary instrumentations.
For the reconstruction of transverse acetabular fractures, different fixation techniques were compared under single-leg stance and sit-to-stand loading. For clinical practice, our results showed that a single plate might provide inadequate stability for transverse fractures and should be complemented by an additional plate or column screw. Furthermore, the strength of acetabular fracture-fixation constructs is overestimated if loading in biomechanical testing is applied only in single-leg stance.
For proximal humerus fractures in patients with compromised bone quality, a mushroom-shaped allograft in combination with a locking plate significantly enhances construct stiffness and failure load and it may therefore be a viable option for the surgical treatment of unstable varus-displaced proximal humerus fractures.
A novel knee joint simulator was designed, built and validated to complement the portfolio of existing joint simulators for in vitro investigations. The knee joint simulator allows active motion of the knee joint with pneumatically controlled artificial muscle models. This setup will enable us to investigate soft tissue injuries and their various reconstruction techniques in the coming years.
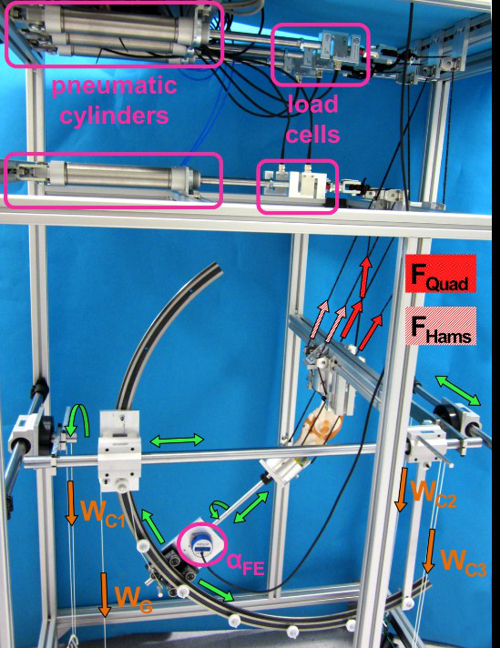
Fig. 1: The novel test bench for the knee joint. Degrees of freedom are labelled in green, applied active muscle forces are labelled in red, passive forces are labelled in orange.
Orthopaedic Biomechanical Gait Laboratory
Dr. Christian Haid
The research of the biomechanical gait laboratory essentially focuses on implementation of the acquired knowledge with the intention of preventing injuries during everyday activity and sport.
Current investigations focus on movement behaviour during daily activity to detect unhealthy loading on the spine. We have conducted several investigations with the aim of understanding the function of the spine and specifically the function of the disc. For these studies, Dr. Haid was honoured with the Volvo award for low back pain research. As a result, we are designing movement patterns to optimise movement from the perspective of health and in the field of maximum power generation in sport.
Morphology and Cell Biology Laboratory
PD Dr.in Ingrid Sitte
Traumatised IVDs of the cervical spine are studied histologically by means of light microscopy and ultrastructurally by means of transmission electron microscopy (TEM). The group is conducting investigations on the basis of two parameters: fracture mechanism (compression vs. rotation fractures) and degeneration grade (low vs. high). Disc architecture is studied histologically; cell morphology is examined ultrastructurally, in order to quantify cell death, healthy cells and balloon cells. Based on ultrastructural observations, two time groups (up to 6 days / longer) are being investigated. Degenerative disc diseases presented a new disc cell morphology, the balloon cell, which we first detected by means of transmission electron microscopy. The aim is to examine this special cell morphology in detail. These cells also seem to be a part of aging processes in the IVD, cartilage and adjacent bone structures. Furthermore, the group is studying intervertebral disc cells in the degenerated cervical spine with prolapse or protrusion and in the cervical spine post-trauma in cell culture, to analyse cell morphology as well as pro-inflammatory and pro-apoptotic proteins with special regard to balloon cells. Whereas these cells were obvious at a mean of 40% in the disc matrix, the cell culture presented up to 98% balloon cells. This may have an influence in an upcoming therapy.
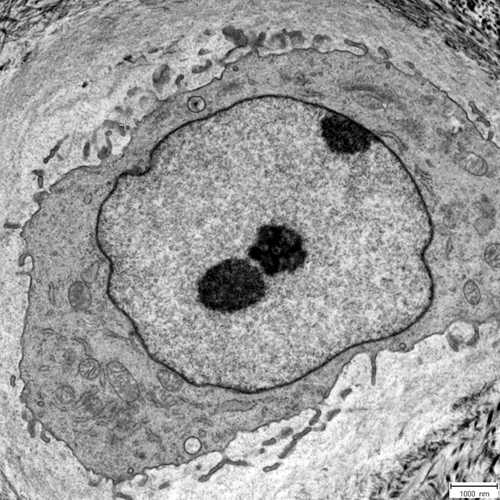
Fig. 2: Balloon cell at 4000x magnification, presenting mostly euchromatin in the nucleus and enveloped by an osmiophilic nuclear membrane
Experimental Orthopaedics
Univ.-Prof. Michael Nogler
The Experimental Orthopaedics unit focuses on translational research. Research and development are initiated by clinical problems. The close link between a strong focus on development and active clinical work together with understanding of the work performed in the daily clinical routine combines new approaches, in order to solve clinical problems. The main directions of research are defined in the microbiological laboratory and the research facilities for computer-aided surgery.
Biofilm Formation and Antimicrobial Susceptibility Tests
Ass. Prof.in Dr.in Deborah Coraça-Huber, PhD, MMSc
Improved understanding of the structure of biofilms and their function helps to develop treatments to avoid attachments and to eliminate biofilms from implant surfaces. The biofilms formed on different surfaces are assessed by comparing the antibiotic susceptibility of different strains and by examining their structures using metabolic and morphological methods.
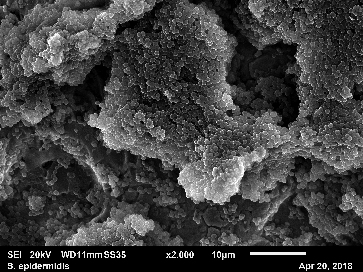
Fig. 3: Biofilm of S. epidermidis formed on a titanium surface
Biofilm-Specific Genes and the Diagnosis of PJIs
Ass. Prof.in Dr.in Deborah Coraça-Huber, PhD, MMSc
A staphylococcal bacterial biofilm is produced in a two-stage process: initial bacterial attachment to the surface of a foreign body or host tissue, followed by biofilm formation comprising bacterial proliferation, intercellular adhesion and extracellular slime substance production. Different genes are involved in each phase of biofilm formation. Although biofilm-specific genes have been investigated, none of this knowledge has been used to develop new PJI diagnostics. These biofilm-specific markers can be detected by means of feasible molecular methods, such as polymerase chain reaction (PCR). Our objective with this research area is to develop a new PCR method by detecting biofilm markers from the joint aspirates of PJI patients.
Osseointegration of Titanium Implants with the Aim of Preventing Biofilm Formation and Peri-Implantitis.
An interdisciplinary project involving dental medicine and orthopaedics has been conducted with the aim of developing a titanium surface that is able to avoid bacterial attachment and biofilm formation. The objective of this study is to evaluate biofilm formation, osteoblast adhesion and the usability of nanostructured Ti13Nb13Zr as well as a conventional Titanium grade 4 alloy with anodised, sol-gel-processed, acid-etched, sandblasted and machined surfaces, with the aim of treating peri-implantitis. The results obtained in this study will be translated into the orthopaedic area.
Simulation of Human Wound and Joint Fluids as Nutrient Media for Biofilm Infection Studies
In this study, the growth and susceptibility of bacterial biofilms are analysed in different nutrient media in comparison with human and in vitro simulated synovial fluids. The aim of this area is to approximate the antimicrobial susceptibility results in the clinical reality. All the results obtained in this area to date by the research society have been achieved with the use of high-nutrient media, which do not normally correspond to the reality of a joint or wound environment.
Natural Antimicrobial Substances
Instead of developing new antibiotics that may display efficacy failure due to resistance mechanisms, there is a need to investigate alternative, antibiotic-boosting substances. Alternative substances can be administrated alone, locally, for the treatment of wound infections and implant infections. In addition, such substances can act as coadjutants, increasing the activity of systemically applied antimicrobials. In this research area, we are investigating the antimicrobial capacity of natural substances, such as omega-3 polyunsaturated fatty acids. This may be an alternative for the treatment of wound and implant infections and for increasing the efficacy of antibiotics that are used systemically.
PD David Putzer, PhD, MSc
The digital operating room is increasingly becoming a reality with the emergence of new technologies, such as augmented reality and robotic assisted surgery. Three-dimensional planning and current visualisation techniques should lead to custom-made, 3D-printed implants and structural allografts on site. In collaboration with the Technical University of Munich, new visualisation techniques for instrument navigation and augmented reality for surgical procedures will be investigated. The visualisation of three-dimensional planning scenarios on remote locations is also the focus of a collaboration with the university of Basel, which aims to introduce a virtual-reality-based planning tool. Together with the University of Rennes, current robot-assisted surgery is being analysed in terms of workflow, ergonomics and efficiency. In a further collaboration led by the Polytechnic University of Turin, a network of doctoral students is being established, which includes several universities, such as the University of Cádiz and the Free University of Brussels, as well as a number of medical device companies. There is also a focus on improving techniques for filling bone defects, with the aim of increasing allograft stability in difficult revision cases. The mechanical properties of allografts have been improved by optimising grain size distribution, liquid content and impaction procedure. Usability and biomechanical investigations have been conducted to improve techniques and instruments for bone removal procedures.
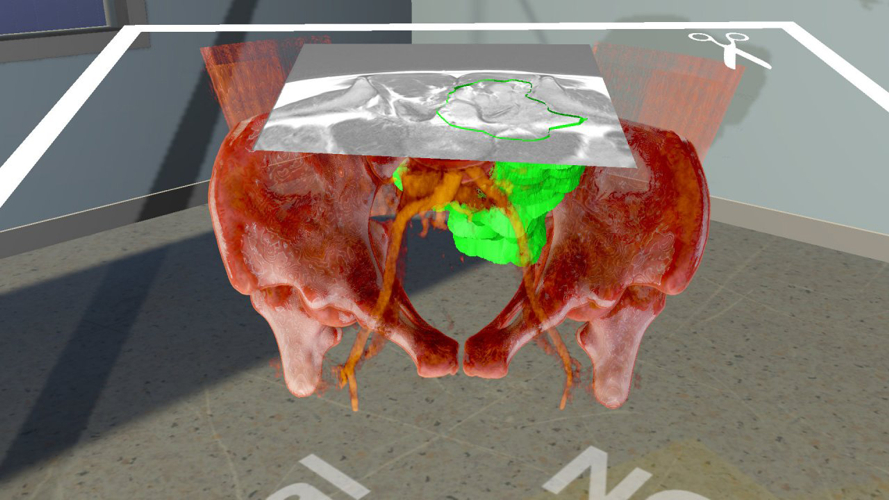
Fig. 4: Three-dimensional visualisation of a tumour case for virtual-reality-assisted planning
Core Facility – Micro CT
PD MMag. Dr. Pallua Johannes PhD
Research applications include fracture healing, skeletal phenotyping, segmental bone defect repair, age-related effects on bone, joint degeneration, tumour infiltration, developmental biology and the microstructure of materials. Both micro-CT scanners can be used for the high-resolution imaging of small animals (ranging from mice to rabbits). The XtremeCT II is also used for high-resolution scanning of patient extremities and primarily for the evaluation of bone density and micro-architecture in the scaphoid bone. The power of these systems lies in their capacity for users to extract quantitative morphometric and density data along with 3D models of their specimens.
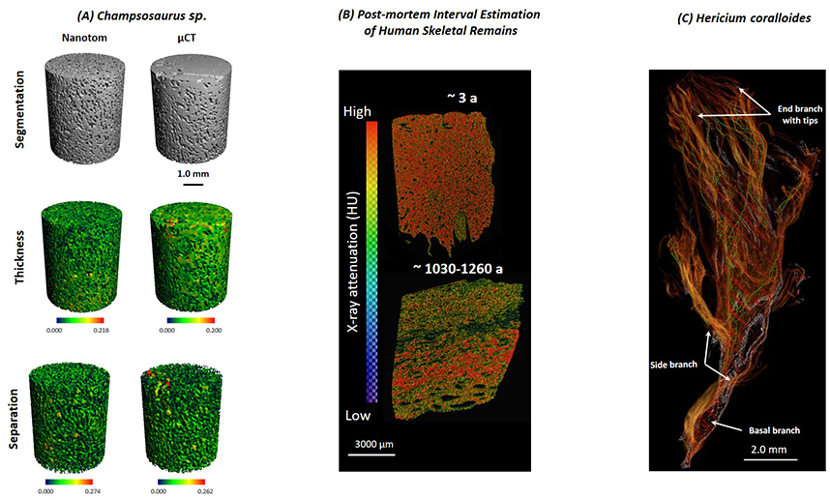
Fig. 5: (A) Comparison of the Structure and Composition of a Fossil Champsosaurus Vertebra with Modern Crocodylidae Vertebrae: A Multi-Instrumental Approach. (B) Post-Mortem Interval Estimation of Human Skeletal Remains by Micro-Computed Tomography, Mid-Infrared Microscopic Imaging and Energy-Dispersive X-Ray Mapping. (C) Application of Micro-Computed Tomography to Microstructure Studies of the Medicinal Fungus Hericium Coralloides.
Selected Publications
- Heike A. Bischoff-Ferrari, MD, DrPH; Bruno Vellas, MD, PhD; René Rizzoli, MD; RetoW. Kressig, MD; José A. P. da Silva, MD, PhD;Michael Blauth, MD; David T. Felson, MD, MPH; Eugene V. McCloskey, MD; BernhardWatzl, PhD; Lorenz C. Hofbauer, MD; Dieter Felsenberg, MD, PhD;Walter C. Willett, MD; Bess Dawson-Hughes, MD; JoAnn E. Manson, MD, DrPH; Uwe Siebert, MD, MPH; Robert Theiler, MD; Hannes B. Staehelin, MD; Caroline de Godoi Rezende Costa Molino, PhD; Patricia O. Chocano-Bedoya,MD, PhD; Lauren A. Abderhalden, PhD; Andreas Egli, MD; John A. Kanis, MD; Endel J. Orav, PhD: Effect of VitaminDSupplementation, Omega-3 Fatty Acid Supplementation, or a Strength-Training Exercise Programon Clinical Outcomes in Older Adults. The DO-HEALTH Randomized Clinical Trial. for the DO-HEALTH Research Group. JAMA: 2020; 324 Nr.18; S.1855-1868
- Kastenberger T, Kaiser P, Schmidle G, Stock K, Benedikt S, Arora R: Clinical results of the BoneWelding®Fiji® anchor for the treatment of Stener lesions of the thumb. Arch Orthop Trauma Surg. 2020 Oct 10. doi: 10.1007/s00402-020-03625-x. Epub ahead of print.
- Liebensteiner MC, Khosravi I, Hirschmann MT, Heuberer PR: Massive cutback in orthopaedic healthcare services due to the COVID-19 pandemic. Board of the AGA-Society of Arthroscopy and Joint-Surgery, Thaler M. Knee Surg Sports Traumatol Arthrosc. 2020 Jun;28(6):1705-1711. doi: 10.1007/s00167-020-06032-2. Epub 2020 Apr 30.
- Lindtner RA, Tiaden AN, Genelin K, Ebner HL, Mancl C, Klawitter M, Sitte I, von Rechenberg B, Blauth M, Richards PJ: Osteoanabolic effect of aldronate and zoledronate on bone marrow stomal cells (BMSCs) isolated from aged osteoporotic patients and its implication for their mode of action in treatment of age-related bone loss. (2014). Osteoporos Int 25(3):1151-61.
- Sitte I, Kathrein A, Klosterhuber M, Lindtner RA, Neururer SB, Rauch S, Kuhn V, Schmölz W: Morphological Similarities after Compression Trauma of Bovine and Human Intervertebral Discs. (2014). Do Disc Cells have a Chance of Surviving? J Orthop Res 32(9): 1198-207.
- Sitte I, Klosterhuber M, Lindtner RA, Freund MC, Neururer SB, Pfaller K, Kathrein A: Morphological changes in the intervertebral disc post trauma: response to fracture-type and degeneration grade. (2016) Eur Spine J. 25(1): 80-95
- Eichinger M, Brunner A, Stofferin H, Bölderl A, Blauth M, Schmölz W: Screw tip augmentation leads to improved primary stability in the minimally invasive treatment of displaced intra-articular fractures of the calcaneus: a biomechanical study. Int Orthop. 2019 Sep;43(9):2175-2181. doi: 10.1007/s00264-018-4171-9. Epub 2018 Oct 10. PMID: 30306219
- Spicher A, Lindtner RA, Zimmermann S, Stofferin H, Schmoelz W: Ultrasound melted polymer sleeve for improved primary pedicle screw anchorage: A novel augmentation technique. Clin Biomech (Bristol, Avon). 2019 Mar;63:16-20. doi: 10.1016/j.clinbiomech.2019.02.007. Epub 2019 Feb 14.
- Heinrichs CH, Knierzinger D, Stofferin H, Schmoelz W: Validation of a novel biomechanical test bench for the knee joint with six degrees of freedom. Biomed Tech (Berl). 2018 Nov 27;63(6):709-717. doi: 10.1515/bmt-2016-0255.
- Kordo Saeed, Alex C. McLaren, Edward M. Schwarz , Valentin Antoci, William V. Arnold, Antonia F. Chen, Martin Clauss, Jaime Esteban, Vanya Gant, Edward Hendershot, Noreen Hickok, Carlos A. Higuera, Débora C. Coraça-Huber, Hyonmin Choe, Jessica A. Jennings, Manjari Joshi, William T. Li, Philip C. Noble, K. Scott Phillips, Paul S. Pottinger, Camilo Restrepo, Holger Rohde, Thomas P. Schaer, Hao Shen, Mark Smeltzer, Paul Stoodle, Jason C. J. Webb, Eivind Witsø: Consensus Paper - 2018 International Consensus Meeting on Musculoskeletal Infection: Summary from the Biofilm Workgroup and Consensus on Biofilm Related Musculoskeletal Infections. Journal Orthopedic Research, Volume 37, Issue5, May 2019, Pages 1007-1017. DOI 10.1002/jor.24229
- Kordo Saeed, Parham Sendi, William V. Arnold, Thomas W. Bauer, Débora C. Coraça!Huber, Antonia F. Che, Hyonmin Choe, John L. Dais, Michelle Ghert, Noreen J. Hicko, Kohei Nishitani, Bryan D. Springer, Paul Stoodley, Thomas P. Sculco, Barry D. Brause, Javad Parvizi, Alex C. McLaren, Edward M. Schwarz: Review – Consensus Statement Paper: Bacterial toxins in musculoskeletal infections. J Orthop Res. 2020;1–11., DOI: 10.1002/jor.24683
- Débora C. Coraça-Huber 1, Lisa Kreidl , Stephan Steixner, Maximilian Hinz, Dietmar Dammerer, Manfred Fille: Research Article - Identification and Morphological Characterization of Biofilms Formed by Strains Causing Infection in Orthopedic Implants. Pathogens 2020, 9, 649; doi:10.3390/pathogens9080649
- Dankl L, Mayr A, Kaufmann G, Thaler M, Nogler M, Putzer D: Measuring bone defects for acetabular revision surgery for choosing an appropriate reconstruction strategy: A concept study on plastic models. Computers in biology and medicine. 2019 Aug 1;103336(111). doi: 10.1016/j.compbiomed.2019.103336.
- Putzer D, Scholl F, Dankl L, Dammerer D, Thaler M, Nogler M: Intraoperative bone defect measurement in the acetabulum using a navigation system: The influence of bone porosity on the digitalization process. Medical engineering & physics. 2018 Sep; 59:75-80. doi: 10.1016/j.medengphy.2018.06.005
- Dammerer D, Putzer D, Glodny B, Petersen J, Arrich F, Krismer M: Occult intra-operative periprosthetic fractures of the acetabulum may affect implant survival. International orthopaedics. 2019 Jul 4;43 (7), 1583-1590. doi: 10.1007/s00264-018-4084-7
- C. Wöss, S. H. Unterberger, G. Degenhart, A. Akolkar, R. Traxl, V. Kuhn, M. Schirmer, A. K. Pallua, R. Tappert, J. D. Pallua: Comparison of Structure and Composition of a Fossil Champsosaurus Vertebra With Modern Crocodylidae Vertebrae: A Multi-Instrumental Approach. J Mech Behav Biomed Mater (2020):104:103668. DOI: 10.1016/j.jmbbm.2020.103668.
- S. Longato, C. Wöss, P. Hatzer-Grubwieser, C. Bauer, W. Parson, S. Unterberger, V. Kuhn, N. Pemberger, A.K. Pallua, W. Recheis, R. Lackner, R. Stalder, J D Pallua: Post-mortem Interval Estimation of Human Skeletal Remains by Micro-Computed Tomography, Mid-Infrared Microscopic Imaging and Energy Dispersive X-ray Mapping. Analytical methods. 02/2015; 7(7). DOI:10.1039/C4AY02943G
- J D Pallua, V. Kuhn, A.F. Pallua, K. Pfaller, A.K. Pallua, W. Recheis, R. Pöder: Application of micro-computed tomography to microstructure studies of the medicinal fungus Hericium coralloides. Mycologia 11/2014; 107(1). DOI:10.3852/14-188
Selection of Funding
Clinical Research:
- Tiroler Wissenschaftsfond – Na-Chlortaurine in ACL
- AO Trauma Austria
- Landesverkehrssicherheitsfond
- AgNovos Healthcare – RESTORE study
- Portola Pharmaceuticals – ANNEXA study
- DePuy Synthes/Jonson&Johnson – musculoskeletal studies
- MAKO procedural study
- Mestex AG – Lopain study
Awards in General:
- Dr. Spicher Anna: Günther-Schlag-Abstractpreis (2020)
- Dr. Runer Armin: ÖGU- Bets Clinical Paper (2019), Sporlactic Poster Award for Clinical Science (2020)
- Dr. Mayr Raul: GOTS-Forschungsförderungspreis (2020)
- Dr. Dammerer: VKO - Vereinigung der Kinderorthopädie der DGOU (2020), Wissenschaftspreis
- Dr. Dammerer: Travelling Fellowship EMSOS-European Musculosceletal Oncologic Society (2019)
- Dr. Thaler: ASG (Austrian Swiss German) Travelling Fellowship (2019)
- Dr. Liebensteiner: Association for Pediatric Orthopedics of Germany- Switzerland-Austria
- Dr. Haid: Volvo Award
Collaborations
Clinical Investigation Unit:
- AO Foundation, Switzerland
- AO Trauma, Austria
- AUVA, Austria
- Prof. Ralph Muller, ETH, Zurich, Switzerland
Biomechanics Laboratory:
- Prof. Dr. med. Tobias Schulte, University of Munster, Germany
- Prof. Ralph Muller, ETH, Zurich, Switzerland
- Prof Dr. med Heiko Koller, TU Munich, Klinikum Rechts der Isar, Germany
- Dr. med. Richard Bostelmann, University of Dusseldorf, DE
- PD Dr. med Stefan Döbele BG Kliniken Tübingen , Germany
- Prof. Dr. med Michael Akbar, Universität Heidelberg, Germany
- PD Dr. med Sven Märdian, Charite, Berlin, Germany
- Prof. Dr. med Andreas Nüssler, Universitätsklinikum Tübingen, Germany
- Prim. Dr. med Vinzenz Smekal, AUVA Klagenfurt
- Alessandro Gasbarrini, MD, Instituto Orthopedico Rizzoli di Bologna, Italy
- Luis Alvarez Galovic, Hospital Universitario Fundacion Jimenez Diaz, Madrid, Spain
Morphology and Cell Biology Laboratory:
- Prof. Charles Archer, University of Cardiff, UK
- Prof. Sally Roberts, Spinal Research, RJAH Orthopaedic Hospital, Oswestry, UK
- Primar Dr. Anton Kathrein, St. Vincenz Krankenhaus, Depart. of Traumatology, Zams
Experimental Orthopedics:
- Origimm GmbH, Wien
- Dr. Johannes Scherer, AdvantIQX, Germany
- Prof. Dr. Eliana A. R. Duek, PUC-Sorocaba, Biomaterials Lab, Brazil
- Prof. Dr. Javad Parvizi, Rothman Institute at Thomas Jefferson University Hospital, Philadelphia, USA
- Prof. Dr. Kordo Saeed, Microbiology Innovation and Research Unit (MIRU), Department of Microbiology, University Hospital Southampton NHS Foundation Trust, University of Southampton School of Medicine, Southampton, UK
- Prof. Dr. Paul Stoodley, Departments of Microbial Infection and Immunity and Orthopedics Infectious Diseases Institute, The Ohio State University, Columbus, Ohio
- Prof. Dr. Philippe C. Cattin, University of Basel, Basel, Switzerland
- Prof. Dr. Nassir Navab, Technical University of Munich, Munich, Germany
- Prof. Christina Bignardi, Politecnico di Torino, Turin, Italy
- Prof. Pierre Jannin, Université de Rennes, Rennes, France
- Prof. Dr. Matthias Harders, University of Innsbruck, Innsbruck, Austria
Devices & Services
Morphology and Cell Biology Laboratory:
- Leica Ultracut R
- Leica DM 6000 B Forschungsmikroskop
- Leica DMI 3000 B Fluoreszenz Mikroskop
Experimental Orthopaedics:
- Scanning electron microscope, JEOL 6010plus
- RT-PCR, PicoReal 96, Thermo Scientifics
- Fluorescence Microscope, Carl Zeiss
 Univ.-Prof. Dr.med.univ. Rohit Arora
Univ.-Prof. Dr.med.univ. Rohit Arora
Director
Contact:
Anichstraße 35
6020 Innsbruck
Austria
Email: Rohit.Arora@i-med.ac.at
Phone: +43 512 504 22821
Fax: +43 512 504 22824
www.ortho-trauma-innsbruck.at



